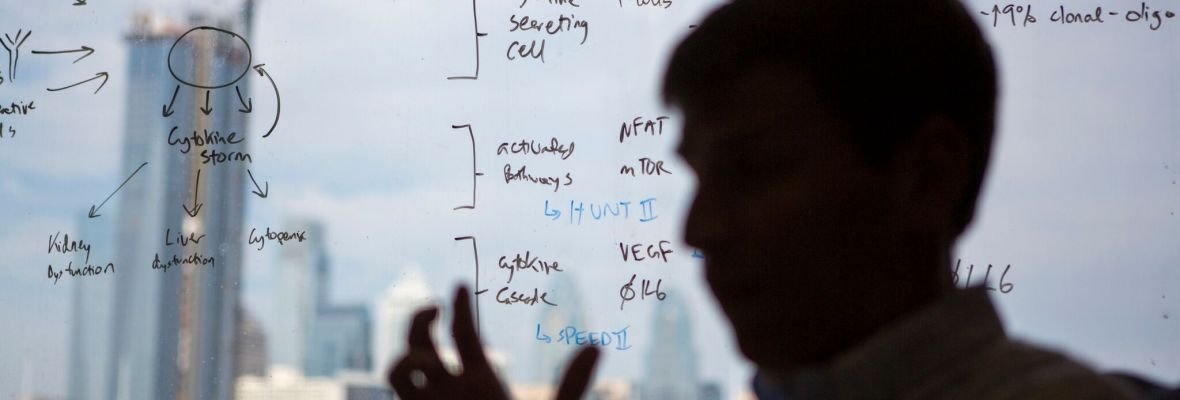
Serum Proteomic Analysis of Cytokine-Driven Entities (SPACE)
What is SPACE?
The Serum Proteomic Analysis of Cytokine-driven Entities (SPACE) study is a multi-site, international, collaborative study to better understand inflammatory disorders and identify novel biomarkers and treatments. We are currently seeking collaborators to contribute approximately 20 125-250-µL already-collected serum samples for the below listing of inflammatory diseases and 5 healthy controls each. We plan to quantify and compare 7,000 serum analytes using Somalogic’s Somascan technology and return the data to collaborators and include them in all publications.
Our Center has utilized serum proteomics to discover novel biomarkers (Pierson et al, Nature Comms, 2022) and treatment approaches (Fajgenbaum et al, JCI, 2019; Pierson et al, Blood Adv, 2021) for idiopathic multicentric Castleman disease. We’re excited to spearhead this collaboration to better understand cytokine storm/cytokine-driven disorders and immunotherapy-induced cytokine storms, which cause significant morbidity and mortality around the world. Few treatment options exist, and limited work has been done to systematically profile cytokine-driven disorders together to identify novel predictive biomarkers, therapeutic targets, or therapeutic approaches.
Goals of SPACE:
To discover novel predictive biomarkers, therapeutic targets, and therapeutic approaches that are shared across and specific to unique cytokine-driven disorders.
Elucidate basic biology of cytokine signaling and immune dysregulation
Click the link below to express interest in contributing samples to this study from various cytokine-driven entities.
See below for additional details.
Using SOMAscan technology to quantify 7,000 protein analytes
We propose to perform a collaborative project to identify diagnostic biomarker(s) and potential novel treatment targets in cytokine release syndromes (CRS). We will utilize our biobank of specimens from expert-graded cases of iMCD as well as related diseases that are on the differential diagnosis with iMCD. We will perform proteomic profiling of 7,000 protein analytes per serum sample using the Somalogic Somascan assay. The Somascan assay allows unbiased target discovery through the use of Slow Off-rate modified aptamer (SOMAmer) technology. Briefly, SOMAmers are able to bind the protein of interest. These protein SOMAmer complexes are then photocleaved and washed. SOMAmers are then hybridized to a microarray and each protein analyte is quantified via fluorescence where fluorescent intensity is proportional to protein quantity in each sample. For more information see below:
Multiplexed SOMAmer affinity assay. (A) SOMAmer reagents labeled with a 5’ fluorophore, photocleavable linker, and biotin are immobilized on streptavidin (SA)-coated beads and incubated with samples containing a complex mixture of proteins. (B) Cognate (top and bottom) and noncognate (middle) SOMAmer–target protein complexes form on the beads. (C) The beads are washed, removing the unbound proteins and the proteins are tagged with biotin. (D) SOMAmer–protein complexes are released from the beads by photocleavage of the linker with UV light. (E) Incubation in a buffer containing a polyanionic competitor selectively disrupts nonspecific interactions. (F) SOMAmer–protein complexes are recaptured on a second set of streptavidincoated beads through biotin-tagged proteins followed by additional washing steps that facilitate further removal of nonspecifically bound SOMAmer reagents. (G) SOMAmer reagents are released from the beads in a denaturing buffer. (H) SOMAmer reagents are hybridized to complementary sequences on a microarray chip and quantified by fluorescence. Fluorescence intensity is related to protein amount in the original sample. (Adapted from Rohloff et al., 2014.)
Research Questions
1) What pre-CRS predictive biomarkers can predict whether a patient will develop CRS upon initiation of cancer immunotherapy?
2) What post-CRS, pre-treatment predictive biomarkers can predict which patients will respond to specific cytokine-directed therapies (anti-IL-6, anti-IL-1, JAKi, etc) once in the midst of a cytokine storm (disease specific and across diseases)?
3) What post-CRS, post-treatment early indicators of response correlate with clinical status and can predict early on whether a patient will go on to respond to cytokine-directed therapies to control a cytokine storm following treatment administration (disease specific and across diseases)?
4) What is the clinical threshold between beneficial inflammation and hyperinflammation?
a. Can we use this threshold to develop an inflammation scale/score to assess how treatments modulate this and whether they are working or not?
b. What are the commonalities and specificities between cytokine-driven disorders?
5) What changes do therapeutic interventions induce within diseases and across diseases over time? What is the remaining disease burden to be addressed with new treatments?
6) What novel therapeutic targets can be identified from quantifying 7,000 serum analytes in patients experiencing cytokine storm (disease specific and across diseases)?
7) What novel treatment approaches can be used to modulate therapeutic targets in patients experiencing cytokine storm (disease specific and across diseases)?
Diseases of Interest and Sample Requirements
Auto-inflammatory:
Idiopathic multicentric Castleman disease (N=60 flare samples)
Hemophagocytic lymphohistiocytosis (N=20 malignancy associated-HLH, N=20 infection associated-HLH, N=20 autoimmunity associated-HLH; N=60)
Vasculitis (N=20)
Kawasaki Disease (n=20)
Undiagnosed inflammatory syndrome/reactive lymphadenopathy (N=20)
Autoimmune:
Systemic lupus erythematosus (N=20 mild/moderate, N=20 severe; N=40)
Crohn’s disease (N=20 mild/moderate, N=20 severe; N=40)
Ulcerative colitis (N=20 mild/moderate, N=20 severe; N=40)
Rheumatoid arthritis (N=20 mild/moderate, N=20 severe; N=40)
Systemic onset Juvenile Idiopathic Arthritis — Still’s Disease (without MAS, so mild/moderate) (N=20)
IgG4 related disease (IgG4RD, N=20)
Sjogren’s Disease (N=20)
Rosai-Dorffman Disease (N=20)
Multisystem high-risk Langerhans cell histiocytosis (N=20)
Pathogen-induced:
COVID19 (N=20 mild/moderate infection, N=20 severe infection, N=20 MIS-A, N=20 PASC; N=80)
Multi-system Inflammatory Syndrome in Children (MIS-C, N=20)
Sepsis (N=20 mild/moderate, N=20 severe; N=40)
Influenza (N=10 mild/moderate infection, N=10 severe infection; N=20)
HHV8-associated multicentric Castleman disease (N=20)
Acute HIV (without HLH) (N=20)
Acute EBV (without HLH) (N=20)
Malignancy-related:
POEMS syndrome (N=20 mild/moderate, N=20 severe, N=10 with longitudinal sample post treatment; N=50)
Hodgkin lymphoma (without HLH) (N=20)
Non-Hodgkin lymphoma (without HLH) (Diffuse large B cell lymphoma; N=20; Angioimmunoblastic T cell lymphoma; N=20)
Follicular lymphoma (N=20) - indolent
Healthy donors:
N~100, 5 healthy donors age-matched and matched to each of the ~20 diseases to address potential site-based pre-analytic variability
Important to have controls from several age points since so many inflammatory cytokines have major changes throughout infancy -> adulthood
Lower priority (but will be considered):
Multiple sclerosis (N=20)
Scleroderma (N=20)
Dengue hemorrhagic fever (N=20)
Post COVID-19 or influenza vaccine with no serious adverse effects (N=20)
Previous Work using SOMAscan proteomic Data
The Center for Cytokine Storm Treatment & Laboratory at the University of Pennsylvania has leveraged SOMAscan to discover the following: A) the first novel drug target for idiopathic multicentric Castleman disease in 25 years (mTOR) (Fajgenbaum et al, JCI, 2019) and validate it in an independent cohort (Arenas et al, Blood, 2020) that led the use of mTOR inhibitors in patients, B) a second novel drug target (JAK1/2) that led to the use of JAK1/2 inhibitors in patients (Chen et al, Lancet, 2021), C) a 7-analyte predictive biomarker of response to anti-IL-6 therapy (Pierson et al, Blood Adv, 2021), and D) discovery of CXCL13, a biomarker measured shortly after initiation of anti-IL-6 therapy that reliably predicts response (Pierson et al, Nature Communications, 2022).
Citations
Pierson SK, Stonestrom AJ, Shilling D, Ruth J, Nabel CS, Singh A, Ren Y, Stone K, Li H, van Rhee F, Fajgenbaum DC. Plasma proteomics identifies a 'chemokine storm' in idiopathic multicentric Castleman disease. Am J Hematol. 2018;93(7):902-912.
Fajgenbaum DC, et al. Identifying and targeting pathogenic PI3K/AKT/mTOR signaling in IL-6-blockade-refractory idiopathic multicentric Castleman disease. J Clin Invest. 2019 Aug 13;129(10):4451-4463.
Arenas DJ, Floess K, Kobrin D, Pai RL, Srkalovic MB, Tamakloe MA, Rasheed R, Ziglar J, Khor J, Parente SAT, Pierson SK, Martinez D, Wertheim GB, Kambayashi T, Baur J, Teachey DT, Fajgenbaum DC. Increased mTOR activation in idiopathic multicentric Castleman disease. Blood. 2020;135(19):1673-1684.
Chen LYC, Skinnider BF, Wilson D, Fajgenbaum DC. Adrenalitis and anasarca in idiopathic multicentric Castleman's disease. Lancet. 2021;397(10286):1749.
Pierson SK, Shenoy S, Oromendia AB, Gorzewski AM, Langan Pai RA, Nabel CS, Ruth JR, Parente SAT, Arenas DJ, Guilfoyle M, Reddy M, Weinblatt M, Shadick N, Bower M, Pria AD, Masaki Y, Katz L, Mezey J, Beineke P, Lee D, Tendler C, Kambayashi T, Fosså A, van Rhee F, Fajgenbaum DC. Discovery and validation of a novel subgroup and therapeutic target in idiopathic multicentric Castleman disease. Blood Adv. 2021;5(17):3445-3456.
Pierson, S. K., Katz, L., Williams, R., Mumau, M., Gonzalez, M., Guzman, S., Rubenstein, A., Oromendia, A. B., Beineke, P., Fosså, A., van Rhee, F., & Fajgenbaum, D. C. (2022). CXCL13 is a predictive biomarker in idiopathic multicentric Castleman disease. Nature Communications, 13(1), 7236.
Rohloff, J. C., Gelinas, A. D., Jarvis, T. C., Ochsner, U. A., Schneider, D. J., Gold, L., & Janjic, N. (2014). Nucleic Acid Ligands With Protein-like Side Chains: Modified Aptamers and Their Use as Diagnostic and Therapeutic Agents. Molecular Therapy. Nucleic Acids, 3(10), e201.


