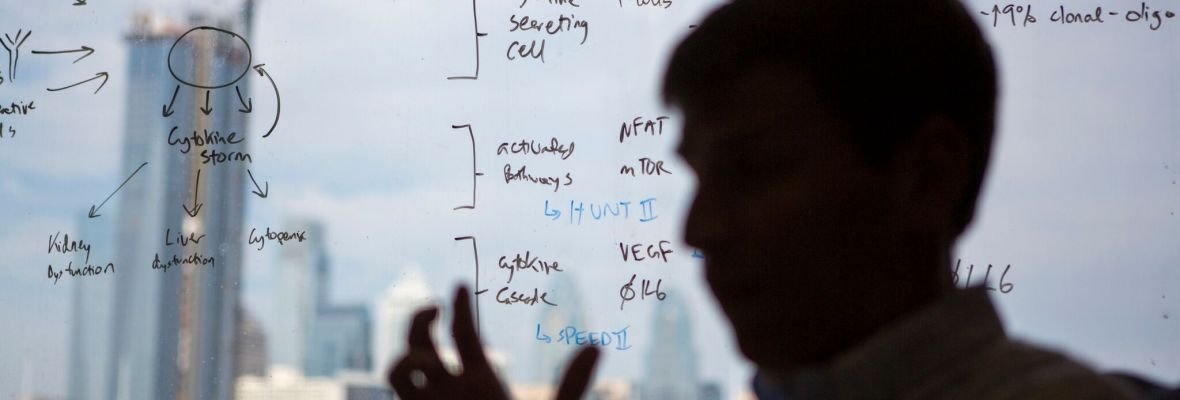
Welcome to the Fajgenbaum Lab, where we work to form a better understanding of Castleman Disease & other Cytokine Storm Disorders
We are recruiting for multiple positions at the CSTL! Check out our current positions here
The Center for Cytokine Storm Treatment & Laboratory (CSTL) [pronounced “Castle”] is dedicated to investigating hyperinflammation and immune system dysregulation in the context of human disease. To gain insight into these types of disorders, our group conducts research with the goal of improving the diagnosis, treatment, and management of Castleman Disease, a rare hyperinflammatory disorder. Our group is unique in that instead of focusing on one experimental technique, or subfield, our lab uses multiple techniques and technologies to study Castleman disease (and other hyperinflammatory disorders) from multiple angles. To fulfill this goal, the CSTL recruits scientists with diverse backgrounds and expertise, including basic bench research, biobanking, and data analysis.
Our interests include:
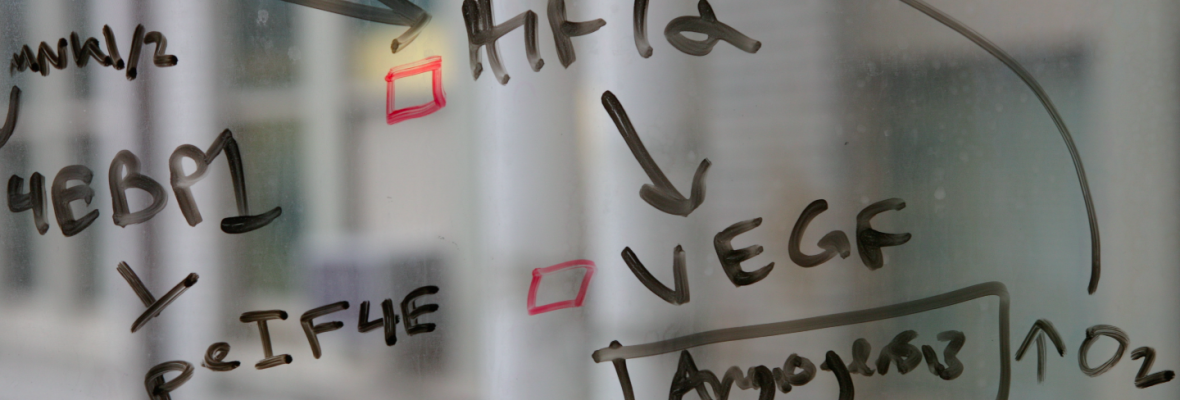
Elucidating the etiology, dysregulated cell types, signaling pathways, and effector cytokines in idiopathic multicentric Castleman disease (iMCD) and related cytokine storm disorders
Identifying effective treatments for iMCD patients
PI3K/Akt/mTOR signaling in iMCD
Understanding the role of stromal cells and chemokines in iMCD.
Our research projects are divided into five broad categories:
Defining CD and its clinico-pathology
Etiology of CD
Pathophysiology
Treatment effectiveness studies
Rare-disease sample acquisition methodologies
Meet the Team
-

David Fajgenbaum, MD, MBA, MSC, FCPP
Founding Director of the Center for Cytokine Storm Treatment & Laboratory
Dr. David Fajgenbaum, MD, MBA, MSc, is an Assistant Professor of Medicine in Translational Medicine & Human Genetics at the University of Pennsylvania, Executive Director of the Castleman Disease Collaborative Network, Associate Director of Patient Impact for the Penn Orphan Disease Center, and national bestselling author of Chasing My Cure: A Doctor's Race to Turn Hope Into Action. He is also a patient battling idiopathic multicentric Castleman disease (iMCD).
-

Joshua Brandstadter, MD, PhD, MSc
Associate Director, Clinical Research
Dr. Joshua Brandstadter is a physician-scientist and Instructor of Medicine in the Division of Hematology/Oncology at the University of Pennsylvania. As Director of Clinical Research for the CSTL, Dr. Brandstadter oversees the ACCERLERATE Natural History Registry to better understand patient experiences and the comparative effectiveness of different treatments. He cares for patients with Castleman Disease in clinic and pursues laboratory research to better understand the causes of the disease. Dr. Brandstadter holds an MSc in Integrated Immunology from the University of Oxford and a combined MD/PhD from Duke University. He completed his internal medicine and hematology/oncology training at the Hospital of the University of Pennsylvania.
-

Melanie Mumau, PhD
Associate Director, Immunology
Melanie Mumau, PhD, is the Associate Director of Immunology at the Center for Cytokine Storm Treatment & Laboratory (CSTL) at the University of Pennsylvania. Melanie is an experimental immunologist by training and oversees all research related to the translational laboratory. She is currently working on understanding the mechanisms that drive cytokine storms and developing new treatments for patients. Melanie earned her PhD in Microbiology & Immunology from Columbia University and prior to joining the CSTL, her research focused on how the immune system regulates the development of blood cells. Melanie enjoys playing soccer, skiing, and making pizza.
-

Michael V. Gonzalez, PhD, MSc
Associate Director, Basic and Translational Research
Mike Gonzalez is the Associate Director of Basic and Translational Research at the Center for Cytokine Storm Treatment and Laboratory (CSTL) within the Perelman School of Medicine at the University of Pennsylvania. He obtained his PhD in Immunology and Infectious Diseases from Washington State University and was a postdoctoral fellow and bioinformatics scientist at the Center for Applied Genomics at the Children’s Hospital of Philadelphia before coming to the CSTL. His research focuses on utilizing novel ’omics technologies to gain insights into the genetic and cellular architectures of Castleman Disease and other disorders involving autoimmunity.
-

Joseph Zinski, PhD
Senior Research Investigator
Joseph Zinski PhD is a Senior Research Investigator at the Center for Cytokine Storm Treatment and Laboratory (CSTL) within the Perelman School of Medicine at the University of Pennsylvania. He received his BS from UConn in Chemical Engineering and his PhD from UPenn in cell and developmental biology. He is using bioinformatic, machine learning, and deep learning to develop better diagnostic tools and treatments for Castleman disease.
-

Abiola Irvine
Research Specialist
Abiola Irvine is a Research Specialist in the Cytokine Storm and Treatment Laboratory at the Perelman School of Medicine. She supports the translational research team in the experimental lab by using immune-based assays and other methods to further our understanding of Castleman Disease. Prior to joining the CSTL team Abiola earned her BS in Psychology with a neuroscience minor from Haverford College and looks forward to applying to medical school in the future. Outside of the lab Abiola enjoys hiking, roller skating, and playing with her dog Hendrxx.
-

Bridget Austin, MS
Biobank Program Manager
Bridget Austin is the Biobank Project Manager for the Center for Cytokine Storm Treatment & Laboratory (CSTL) at the University of Pennsylvania. As such, Bridget works as a clinical liaison between the research and clinical sides of the CSTL, assists with various research projects such as the ACCELERATE Natural History Registry, and coordinates biological sample donation to the CSTL's Castlebank. Bridget earned her MS in Psychology from Villanova University.
-

Mateo Sarmiento Bustamante
Senior Data Analyst
Mateo Sarmiento is a Senior Data Analyst for the Center for Cytokine Storm Treatment & Laboratory (CSTL) at the Perelman School of Medicine. He synthesizes and analyzes information across a Castleman patient’s medical history to gain insight on things such as the wide spectrum of symptoms and the effectiveness of treatment regimens that Castleman patients experience. Mateo looks forward to spending his gap years at the CSTL before applying to medical school. Prior to joining the CSTL, Mateo earned his BA in Neuroscience at the University of Pennsylvania where he researched the epigenetics of drug addiction.
-

Saishravan Shyamsundar
Data Analyst
Saishravan Shyamsundar is a Data Analyst for the Center for Cytokine Storm & Treatment Laboratory (CSTL) at Perelman School of Medicine. He earned a Bachelor of Science in Biomedical Engineering from Rensselaer Polytechnic Institute and a Master of Science in Biomedical Sciences from Geisinger Commonwealth School of Medicine. At CSTL, he supports the ACCELERATE Registry Team (ART) in data compilation and analysis of medical records of Castleman Disease patients. The analysis of this data could then provide further insights into understanding the mechanisms of the disease and identifying effective treatment options. He hopes that his work with this team helps lead to better prognosis for patients with Castleman Disease
-

Larissa Borys
Clinical Research Coordinator
Larissa Borys is a Clinical Research Coordinator for the Center for Cytokine Storm Treatment & Laboratory (CSTL) at the University of Pennsylvania. She supports the ACCELERATE Natural History Registry and works closely with the CSTL’s Castlebank to ensure proper data compilation of the diagnosis and treatment processes for patients with Castleman Disease. Prior to joining the CSTL, Larissa researched biomarker discovery and development for neurodegenerative diseases at Columbia University Irving Medical Center. She earned her BA in Neuroscience at the University of Pennsylvania. Larissa will be working at the CSTL before applying to medical school.n goes here
-

Amber Vas
Executive Administrator
Amber Vas is the Executive Administrator for the Center for Cytokine Storm Treatment & Laboratory (CSTL) at the Perelman School of Medicine. She provides direct support for the Director of the CSTL and overseas the administrative functions of the CSTL’s various projects and events. Prior to her work for the CSTL, Amber was the executive coordinator for the Department of Biostatics, Epidemiology, and Informatics and the Center for Health Behavior Research. Amber earned her BA in Psychology from the University of Richmond.
-

Payton Morrissey
Executive Assistant
Payton Morrissey is the Executive Assistant to David Fajgenbaum, MD, MBA, MSc at the Cytokine Storm Treatment & Laboratory (CSTL) at the Perelman School of Medicine. She provides direct support to the Director of the CSTL and oversees calendar management and the coordination of travel and events. Prior to joining the CSTL, Payton was a cybersecurity consultant and media coordinator for a cybersecurity firm. She graduated with her B.S. in Security and Risk Analysis from the College of Information Sciences and Technology at Penn State University.
-
Divyaraj Singh Nirwan
Biobank Assistant
Divyaraj Nirwan is the Biobank assistant for Centre for Cytokine Storm Treatment & Laboratory (CSTL) and helps in expanding its sample biobank (Castlebank) and collaborates with members of the translational team on various tasks. He is a dedicated and skilled biotechnologist with a strong academic background in bioinformatics, pursuing his master of biotechnology at the University of Pennsylvania. He has diverse experience in quality control and innovative research projects. His expertise spans a wide range of technical and software skills, complemented by his strong organizational abilities and commitment to academic and community initiatives.
Former Lab Members and Alumni
Tracey Sikora. Currently Vice President of Research & Clinical Programs at National Organization for Rare Disorders (NORD).
Criswell Lavery, MPH. Project Manager & Health Research Specialist at the Corporal Michael J. Crescenz VA Medical Center.
Sheila Pierson, MS. Currently a medical student at Temple University School of Medicine
Natalie Mango. Currently a medical student at the Perleman School of Medicine at the University of Pennsylvania
Jasira Ziglar, MD, MPH. Currently a resident in Internal Medicine at University of Massachusetts.
Helen Partridge, MD. Currently a resident in psychiatry at Perelman School of Medicine.
Dustin Shilling, PhD. Currently a senior associate at Spark Therapeutics.
Faizaan Ahkter, DO. Currently a resident in internal medicine at Rowan University.
Erin Napier, MD. Currently a resident in ophthalmology at UCLA Jules Stein Eye Institute.
Alexander Suarez, MD. Currently a resident in neurosurgery at Duke School of Medicine.
Dale Kobrin, MD. Currently a resident in internal medicine at Allegheny General Hospital.
Eric Haljasmaa. Currently a medical student at Lake Erie College of Osteopathic Medicine.
Katherine Floess, MD. Currently a resident of internal medicine at Montefiore Medical Center.
Sophia Parente, MD. Currently a resident of internal medicine at the University of Minnesota.
Mark-Avery Tamakloe. Currently a medical student at Rutgers Robert Wood Johnson Medical School.
Victoria (Tori) Powers. Currently a medical student at Sidney Kimmel Medical College.
Alexander (Alek) Gorzewski. Currently a medical student at Northwestern University Feinberg School of Medicine.
Rozena Rasheed. Currently central laboratory specialist for portfolio sourcing and relationship management at Merck Pharmaceuticals.
Alexis Phillips, MD. Currently a resident in internal medicine at Massachusetts General Hospital.
Ruth-Anne Pai, PhD. Currently a Chief Scientific Consultant at Pai Advisory, LLC.
Johnson Khor, MCHI. Currently a medical student at the University of Queensland-Ochsner Clinical School.
Hemi Park, MPH. Currently a program manager at Massachusetts General Hospital
Freda Coren. Currently a medical student at the University of Texas at Austin.
Reece Williams. Currently a medical student at Emory University.
Daniel Arenas, PhD. Currently a resident in pathology at Stanford University.

We are always looking for talented individuals to join the lab!
What is a Cytokine Storm?
A cytokine storm occurs when the body releases too many cytokines into the blood too quickly causing a severe immune reaction. Cytokines are an important part of a normal immune response, but can be extremely harmful when a large amount of them are released into the body. A cytokine storm can occur as a result of an infection, autoimmune condition, or other disease. Signs and symptoms of a cytokine storm can include high fever, inflammation (redness and swelling), severe fatigue and nausea. Sometimes, a cytokine storm may be severe or life threatening and lead to multiple organ failure as seen in the most severe cases of Castleman disease.
What is Castleman disease?
Overview
Castleman disease (CD) describes a group of rare disorders that involve enlarged lymph nodes with a similar lymph node appearance under the microscope and a broad range of inflammatory symptoms and laboratory abnormalities. There are four main subtypes of CD:
Unicentric Castleman disease (UCD)
POEMS-associated multicentric Castleman disease (POEMS-MCD)
HHV-8-associated multicentric Castleman disease (HHV-8+MCD)
HHV-8-negative/idiopathic multicentric Castleman disease (iMCD)
Disease overview
Castleman disease (CD) describes a group of rare disorders that involve enlarged lymph nodes and a broad range of inflammatory symptoms and laboratory abnormalities. The lymph nodes, and the cells that reside in them (lymphocytes and stromal cells), are an integral part of our immune system that help us fight invading organisms and cancer. In a healthy individual, the cells of the immune system become activated to fight off invading organisms or cancer and then return to a surveillance mode. In CD, the cells of the immune system become hyper-activated, overproduce cytokines and other inflammatory compounds, and fail to return to a surveillance mode.
Approximately 4,300-5,200 cases of CD are diagnosed in the US each year; CD can occur in people of any age, gender, or ethnicity. All forms of CD involve a constellation of microscopic abnormalities in the lymph node tissue that can be observed following a lymph node biopsy. Whether Castleman disease should be considered an autoimmune disease, cancer, or infectious disease is currently unknown. The symptoms, causes, and treatments vary greatly for each subtype of CD.
Learn more about the signs and symptoms of Castleman disease here.
Learn more about diagnosing and treating Castleman disease here.
Cytokine Storm and Castleman disease
Castleman disease patients in flare experience a hyper-response from their immune system. This cytokine storm in their bodies causes immune dysregulation characterized by constitutional symptoms, systemic inflammation, multi-organ dysfunction that can lead to multi-organ failure, and in the most severe cases, even death.
Castleman disease patients with the most severe subtype (iMCD TAFRO) suffer from thrombocytopenia, anasarca, fever, reticulin fibrosis, and organomegaly and have the most severe cytokine storms. Patients with iMCD have no known cause of their disease but interleukin-6 is the driver of pathogenesis in a large portion of patients.
First-line treatment for idiopathic multicentric Castleman disease is anti-IL-6 therapy with siltuximab (or tocilizumab, if siltuximab is not available). Siltuximab (Sylvant) is the only FDA-approved treatment for iMCD and patients who responded to siltuximab tend to have long-term responses. This drug targets a specific protein (interleukin-6) that is highly involved in inflammation. Unlike traditional chemotherapy, anti-IL6 therapy is more targeted and doesn’t result in the elimination of any cell types so the side effects are milder.
For patients who do not respond to first line therapy, the CSTL has worked to uncover several other treatment approaches in CD including:
Siltuximab for iMCD - supported the initial approval, recommend it first line in guidelines, and have continued to support this through running a study to help maintain its approval in Europe
Sirolimus for iMCD - discovered that sirolimus may be effective, treated patients effectively, and launched a clinical trial. Learn more about this trial here.
Ruxolitinib for iMCD - discovered that ruxolitinib may be effective, treated patients effectively, and launched a clinical trial
Rituximab for iMCD - collaborated on a retrospective study indicating that it can be used as a second or third line treatment
Velcade-dexamethasone-thalidomide - collaborated on a clinical trial indicating that it can be used as a second or third line treatment
Thalidomide-cyclophosphamide-prednisone - collaborated on a clinical trial indicating that it can be used as a second or third line treatment
Other potential drugs identified from our research that need further investigation:
Siltuximab for unresectable UCD
Rituximab for unresectable UCD
Embolization for unresectable UCD
Eculizumab for iMCD
Trametinib for iMCD
Sapanisertib for iMCD
Anti-CXCL13/CXCR5 therapies for iMCD
You can learn more about the Diagnostic criteria and treatment guidelines for iMCD here.
Relevant publications:
-
Scientists at the CSTL published the first ever consensus of iMCD diagnosis guidelines found here. Our ongoing natural history research powered by our ACCELERATE database will allow us to test and improve these guidelines further.
For more information, click here.
-
The cause of hyper-activation of the immune system in iMCD is still unknown. One of the main hypotheses is that an infectious agent, such as a virus or bacteria, triggers the immune system. Our lab is using multiple methods to study lymph node tissue of iMCD patients in order to search for the DNA of viruses, fungi, and bacteria.
For more information, click here.
-
Proteomic quantification of serum samples is allowing us to biochemically characterize the heterogeneity of iMCD and how it fits with other related diseases such as rheumatoid arthritis and Hodgkin lymphoma. Serum analytes may also lead to the development of algorithms that predict which patients would respond to specific treatments (such as IL-6 blockade). Furthermore, serum proteins may signal the hyperactivation of certain biochemical pathways and elucidate them as novel therapeutic targets.
For more information, click here.
-
Human herpesvirus (HHV)-8-negative, idiopathic multicentric Castleman disease (iMCD) is a deadly hematologic illness involving progressive flares of systemic inflammation, polyclonal lymphoproliferation, and multiple organ system dysfunction. Approximately 600-1000 individuals of all ages are diagnosed annually in the USA; 35% die within 5 years. Poor outcomes are related to the limited mechanistic understanding of iMCD. The etiology, dysregulated signaling pathway, and cell type in iMCD are completely unknown. A family with germline FAS mutations in a patient with iMCD and one with UCD has been reported, however very limited research has been performed into genetic risk factors and/or pathogenic variants
For more information, click here.
-
We know that CD is a heterogeneous group of disorders involving systemic inflammation and polyclonal lymphoproliferation, and it is important to note that there are no clonal cell populations that are visible microscopically and no evidence of spreading or “metastasis,” which is often the case with somatically-mutated/clonal malignancies. Nevertheless, given the clinico-pathologic similarities between iMCD and disorders like Hodgkin lymphoma and angioimmunoblastic T-cell lymphoma, the field has long hypothesized that a rare population of somatically mutated clonal cells may be involved in UCD and iMCD pathogenesis. Recently, somatic mutations have been described in a couple studies of unclear/poor quality in patients with UCD and iMCD, suggesting a potential role for somatically mutated cells in pathogenesis.
For more information, click here.
-
In iMCD we still don't know which immune cells or pathways are activated. This study looks for the activated immune cells and cellular pathways. We are examining iMCD lymph node tissue using multiple cutting-edge technologies, such as TCRb sequencing, BCR sequencing, flow cytometry, Whole Exome Sequencing, CyTOF, MIBI, CODEX, and/or single-cell RNASeq. These new technologies will investigate dozens and hundreds of markers to help determine the active cell types and cellular pathways.
For more information, click here.
-
Idiopathic multicentric Castleman disease (iMCD) is a heterogeneous cytokine storm disorder that involves systemic inflammation, multicentric lymphadenopathy with characteristic histopathology, and life-threatening multiple organ dysfunction. Patients can present with a range of symptoms from thrombocytopenia, anasarca, fever/elevated C-reactive protein (CRP), reticulin myelofibrosis, renal dysfunction, and organomegaly (iMCD-TAFRO) to thrombocytosis, hypergammaglobulinemia, and plasmacytosis (iMCD-IPL); patients not falling into either group are considered iMCD-NOS. Though the etiology of iMCD is unknown, the proinflammatory cytokine interleukin-6 (IL-6) drives disease pathogenesis in a portion of patients. Unfortunately, two-thirds of patients do not respond to anti-IL-6 therapy, the only FDA-approved treatment, and limited treatments exist beyond anti-IL-6 therapy due to poor understanding of pathogenesis. The molecular mechansims of iMCD, particularly within the three clinical subtypes and compared to clinco-pathologically overlapping inflammatory disorders has not been elucidated. Here, we report our findings characterizing quantitative gene expression data using multiple platforms on lymph node tissue from iMCD, pathologically related disorders, and normal controls. The transcriptome of iMCD-TAFRO lymph node tissue identified a number of significantly altered genes involved in angiogenesis, cell proliferation, and orchestration of multiple facets of the humoral and innate immune response. Gene expression data revealed shared upregulation of multiple genes across clinical subtypes of iMCD, supporting a role for shared pathologic mechanisms across iMCD subtypes.
For more information, click here.
-
Neutrophil extracellular traps (NETs) are net-like structures composed of DNA-histone complexes that are released by activated neutrophils, usually in response to bacteria, fungi, or viruses. NETs can be induced by auto-antibodies, and NETs are capable of inducing potent IFN-I production by plasmacytoid dendritic cells and thus a strong IFN-I response in other cells. Increasing evidence suggests that NETs play an important role in autoimmunity including SLE and RA. The purpose of this study is to determine if NETs play a role in the pathogenesis/etiology of iMCD and to gain an initial indication of the potential role of neutrophils in the inflammatory/immune response in iMCD.
For more information, click here.
-
Castleman Disease (CD) is a rare, atypical lymphoproliferative disorder with significant morbidity and mortality and a poorly understood pathophysiology. Defined by a shared lymph node (LN) histology, CD encompasses a wide range of clinical presentations from unifocal adenopathy with mild symptoms (unicentric CD, UCD) to multifocal adenopathy with a systemic inflammatory cytokine storm driving multi-organ dysfunction (multicentric CD, MCD). MCD can be further divided into human herpesvirus (HHV)-8-associated MCD and HHV-8-negative/idiopathic MCD (iMCD). Disease etiology, pathophysiology, including the identity of the pathogenic cells and transcriptional programs, remains largely unknown. Thus, a fundamental question in CD is whether an etiological mechanism of iMCD is an infectious disease, an inflammatory disease, or an autoimmune disease. In this study, we hypothesized that autoantibodies may be driving iMCD pathology in at least a subset of iMCD patients.
For more information, click here.
Research Projects
Serum Proteomic Analysis of Cytokine-Driven Entities (SPACE)
What is SPACE?
The Serum Proteomic Analysis of Cytokine-driven Entities (SPACE) study is a multi-site, international, collaborative study to better understand inflammatory disorders and identify novel biomarkers and treatments. We are currently seeking collaborators to contribute approximately 20 125-250-µL already-collected serum samples for the below listing of inflammatory diseases and 5 healthy controls each. We plan to quantify and compare 7,000 serum analytes using Somalogic’s Somascan technology and return the data to collaborators and include them in all publications.
Our Center has utilized serum proteomics to discover novel biomarkers (Pierson et al, Nature Comms, 2022) and treatment approaches (Fajgenbaum et al, JCI, 2019; Pierson et al, Blood Adv, 2021) for idiopathic multicentric Castleman disease. We’re excited to spearhead this collaboration to better understand cytokine storm/cytokine-driven disorders and immunotherapy-induced cytokine storms, which cause significant morbidity and mortality around the world. Few treatment options exist, and limited work has been done to systematically profile cytokine-driven disorders together to identify novel predictive biomarkers, therapeutic targets, or therapeutic approaches.
Goals of SPACE:
To discover novel predictive biomarkers, therapeutic targets, and therapeutic approaches that are shared across and specific to unique cytokine-driven disorders.
Elucidate basic biology of cytokine signaling and immune dysregulation
Click the link below to express interest in contributing samples to this study from various cytokine-driven entities.
See below for additional details.
Using SOMAscan technology to quantify 7,000 protein analytes
We propose to perform a collaborative project to identify diagnostic biomarker(s) and potential novel treatment targets in cytokine release syndromes (CRS). We will utilize our biobank of specimens from expert-graded cases of iMCD as well as related diseases that are on the differential diagnosis with iMCD. We will perform proteomic profiling of 7,000 protein analytes per serum sample using the Somalogic Somascan assay. The Somascan assay allows unbiased target discovery through the use of Slow Off-rate modified aptamer (SOMAmer) technology. Briefly, SOMAmers are able to bind the protein of interest. These protein SOMAmer complexes are then photocleaved and washed. SOMAmers are then hybridized to a microarray and each protein analyte is quantified via fluorescence where fluorescent intensity is proportional to protein quantity in each sample. For more information see below:
Multiplexed SOMAmer affinity assay. (A) SOMAmer reagents labeled with a 5’ fluorophore, photocleavable linker, and biotin are immobilized on streptavidin (SA)-coated beads and incubated with samples containing a complex mixture of proteins. (B) Cognate (top and bottom) and noncognate (middle) SOMAmer–target protein complexes form on the beads. (C) The beads are washed, removing the unbound proteins and the proteins are tagged with biotin. (D) SOMAmer–protein complexes are released from the beads by photocleavage of the linker with UV light. (E) Incubation in a buffer containing a polyanionic competitor selectively disrupts nonspecific interactions. (F) SOMAmer–protein complexes are recaptured on a second set of streptavidincoated beads through biotin-tagged proteins followed by additional washing steps that facilitate further removal of nonspecifically bound SOMAmer reagents. (G) SOMAmer reagents are released from the beads in a denaturing buffer. (H) SOMAmer reagents are hybridized to complementary sequences on a microarray chip and quantified by fluorescence. Fluorescence intensity is related to protein amount in the original sample. (Adapted from Rohloff et al., 2014.)
Research Questions
1) What pre-CRS predictive biomarkers can predict whether a patient will develop CRS upon initiation of cancer immunotherapy?
2) What post-CRS, pre-treatment predictive biomarkers can predict which patients will respond to specific cytokine-directed therapies (anti-IL-6, anti-IL-1, JAKi, etc) once in the midst of a cytokine storm (disease specific and across diseases)?
3) What post-CRS, post-treatment early indicators of response correlate with clinical status and can predict early on whether a patient will go on to respond to cytokine-directed therapies to control a cytokine storm following treatment administration (disease specific and across diseases)?
4) What is the clinical threshold between beneficial inflammation and hyperinflammation?
a. Can we use this threshold to develop an inflammation scale/score to assess how treatments modulate this and whether they are working or not?
b. What are the commonalities and specificities between cytokine-driven disorders?
5) What changes do therapeutic interventions induce within diseases and across diseases over time? What is the remaining disease burden to be addressed with new treatments?
6) What novel therapeutic targets can be identified from quantifying 7,000 serum analytes in patients experiencing cytokine storm (disease specific and across diseases)?
7) What novel treatment approaches can be used to modulate therapeutic targets in patients experiencing cytokine storm (disease specific and across diseases)?
Diseases of Interest and Sample Requirements
Auto-inflammatory:
Idiopathic multicentric Castleman disease (N=60 flare samples)
Hemophagocytic lymphohistiocytosis (N=20 malignancy associated-HLH, N=20 infection associated-HLH, N=20 autoimmunity associated-HLH; N=60)
Vasculitis (N=20)
Kawasaki Disease (n=20)
Undiagnosed inflammatory syndrome/reactive lymphadenopathy (N=20)
Autoimmune:
Systemic lupus erythematosus (N=20 mild/moderate, N=20 severe; N=40)
Crohn’s disease (N=20 mild/moderate, N=20 severe; N=40)
Ulcerative colitis (N=20 mild/moderate, N=20 severe; N=40)
Rheumatoid arthritis (N=20 mild/moderate, N=20 severe; N=40)
Systemic onset Juvenile Idiopathic Arthritis — Still’s Disease (without MAS, so mild/moderate) (N=20)
IgG4 related disease (IgG4RD, N=20)
Sjogren’s Disease (N=20)
Rosai-Dorffman Disease (N=20)
Multisystem high-risk Langerhans cell histiocytosis (N=20)
Pathogen-induced:
COVID19 (N=20 mild/moderate infection, N=20 severe infection, N=20 MIS-A, N=20 PASC; N=80)
Multi-system Inflammatory Syndrome in Children (MIS-C, N=20)
Sepsis (N=20 mild/moderate, N=20 severe; N=40)
Influenza (N=10 mild/moderate infection, N=10 severe infection; N=20)
HHV8-associated multicentric Castleman disease (N=20)
Acute HIV (without HLH) (N=20)
Acute EBV (without HLH) (N=20)
Malignancy-related:
POEMS syndrome (N=20 mild/moderate, N=20 severe, N=10 with longitudinal sample post treatment; N=50)
Hodgkin lymphoma (without HLH) (N=20)
Non-Hodgkin lymphoma (without HLH) (Diffuse large B cell lymphoma; N=20; Angioimmunoblastic T cell lymphoma; N=20)
Follicular lymphoma (N=20) - indolent
Healthy donors:
N~100, 5 healthy donors age-matched and matched to each of the ~20 diseases to address potential site-based pre-analytic variability
Important to have controls from several age points since so many inflammatory cytokines have major changes throughout infancy -> adulthood
Lower priority (but will be considered):
Multiple sclerosis (N=20)
Scleroderma (N=20)
Dengue hemorrhagic fever (N=20)
Post COVID-19 or influenza vaccine with no serious adverse effects (N=20)
Previous Work using SOMAscan proteomic Data
The Center for Cytokine Storm Treatment & Laboratory at the University of Pennsylvania has leveraged SOMAscan to discover the following: A) the first novel drug target for idiopathic multicentric Castleman disease in 25 years (mTOR) (Fajgenbaum et al, JCI, 2019) and validate it in an independent cohort (Arenas et al, Blood, 2020) that led the use of mTOR inhibitors in patients, B) a second novel drug target (JAK1/2) that led to the use of JAK1/2 inhibitors in patients (Chen et al, Lancet, 2021), C) a 7-analyte predictive biomarker of response to anti-IL-6 therapy (Pierson et al, Blood Adv, 2021), and D) discovery of CXCL13, a biomarker measured shortly after initiation of anti-IL-6 therapy that reliably predicts response (Pierson et al, Nature Communications, 2022).
Citations
Pierson SK, Stonestrom AJ, Shilling D, Ruth J, Nabel CS, Singh A, Ren Y, Stone K, Li H, van Rhee F, Fajgenbaum DC. Plasma proteomics identifies a 'chemokine storm' in idiopathic multicentric Castleman disease. Am J Hematol. 2018;93(7):902-912.
Fajgenbaum DC, et al. Identifying and targeting pathogenic PI3K/AKT/mTOR signaling in IL-6-blockade-refractory idiopathic multicentric Castleman disease. J Clin Invest. 2019 Aug 13;129(10):4451-4463.
Arenas DJ, Floess K, Kobrin D, Pai RL, Srkalovic MB, Tamakloe MA, Rasheed R, Ziglar J, Khor J, Parente SAT, Pierson SK, Martinez D, Wertheim GB, Kambayashi T, Baur J, Teachey DT, Fajgenbaum DC. Increased mTOR activation in idiopathic multicentric Castleman disease. Blood. 2020;135(19):1673-1684.
Chen LYC, Skinnider BF, Wilson D, Fajgenbaum DC. Adrenalitis and anasarca in idiopathic multicentric Castleman's disease. Lancet. 2021;397(10286):1749.
Pierson SK, Shenoy S, Oromendia AB, Gorzewski AM, Langan Pai RA, Nabel CS, Ruth JR, Parente SAT, Arenas DJ, Guilfoyle M, Reddy M, Weinblatt M, Shadick N, Bower M, Pria AD, Masaki Y, Katz L, Mezey J, Beineke P, Lee D, Tendler C, Kambayashi T, Fosså A, van Rhee F, Fajgenbaum DC. Discovery and validation of a novel subgroup and therapeutic target in idiopathic multicentric Castleman disease. Blood Adv. 2021;5(17):3445-3456.
Pierson, S. K., Katz, L., Williams, R., Mumau, M., Gonzalez, M., Guzman, S., Rubenstein, A., Oromendia, A. B., Beineke, P., Fosså, A., van Rhee, F., & Fajgenbaum, D. C. (2022). CXCL13 is a predictive biomarker in idiopathic multicentric Castleman disease. Nature Communications, 13(1), 7236.
Rohloff, J. C., Gelinas, A. D., Jarvis, T. C., Ochsner, U. A., Schneider, D. J., Gold, L., & Janjic, N. (2014). Nucleic Acid Ligands With Protein-like Side Chains: Modified Aptamers and Their Use as Diagnostic and Therapeutic Agents. Molecular Therapy. Nucleic Acids, 3(10), e201.
Select Publications
2024
Sarmiento Bustamante, M., Pierson, S.K., Ren, Y., Bagg, A., Brandstadter, J.D., Srkalovic, G., Mango, N., Alapat, D., Lechowicz, MJ., Li, H., van Rhee, F., Lim, M.S., & Fajgenbaum, D.C. (2024). Longitudinal, natural history study reveals the disease burden of idiopathic multicentric Castleman disease. Haematologica, online ahead of print. https://doi.org/10.3324/haematol.2023.283603
Rubenstein, A.I., Pierson, S.K., Shyamsundar, S., Sarmiento Bustamante, M., Gonzalez, M.V., Milller, I.D., Brandstadter, J.D., Mumau, M.D., & Fajgenbaum, D.C. (2024). Immune-mediated thrombocytopenia and IL-6-mediated thrombocytosis observed in idiopathic multicentric Castleman disease. British Journal of Haematology, online ahead of print. https://doi.org/10.1111/bjh.19279
2023
Sarmiento Bustamante, M., Shyamsundar, S., Coren, F.R., Adam Bagg, A., Srkalovic, G., Alapat, D., van Rhee, F., Lim, M.S., Lechowicz, MJ., Brandstadter, J.D., Pierson, S.K., & Fajgenbaum, D.C. (2023). Ongoing symptoms following complete surgical excision in unicentric Castleman disease." American Journal of Hematology, 98(11), E334-E337. https://doi.org/10.1002/ajh.27065
Korsunska, A., Repasky, M., Zuccato, M., & Fajgenbaum, D.C. (2023). A model for crowdsourcing high-impact research questions for Castleman disease and other rare diseases. Orphanet Journal of Rare Disease, 18(1), 75. https://doi.org/10.1186/s13023-023-02678-6
Pierson, S.K., Lim, M.S., Srkalovic, G., Brandstadter, J.D., Sarmiento Bustamante, M., Shyamsundar, S., Mango, N., Lavery, C., Austin, B., Alapat, D., Lechowicz, MJ., Bagg, A., Li, H., 8, Casper, C., van Rhee, F., & Fajgenbaum, D.C. (2023). Treatment consistent with idiopathic multicentric Castleman disease guidelines is associated with improved outcomes. Blood Advances, 7(21): 6652-6664. https://doi.org/10.1182/bloodadvances.2023010745
Mango, N.A., Pierson, S.K., Sarmiento Bustamante, M., Brandstadter, J.D., van Rhee, F., & Fajgenbaum, D.C. (2023) Siltuximab administration results in spurious IL-6 elevation in peripheral blood. American Journal of Hematology. 99(1); E15-E18. https://doi.org/10.1002/ajh.27132
Horna, P., King. R.L., Jevremovic, D., Fajgenbaum, D.C., & Dispenzieri, A. (2023). The lymph node transcriptome of unicentric and idiopathic multicentric Castleman disease. Haematologica, 108(1), 207-218. https://doi.org/10.3324/haematol.2021.280370
Rodolfi, S., Della-Torre, E., Bongiovanni, L., Mehta, P., Fajgenbaum, D.C., & Carlo Selmi, C. (2023) Lymphadenopathy in the rheumatology practice: a pragmatic approach. Rheumatology (Oxford). kead644. https://doi.org/10.1093/rheumatology/kead644
Brandstadter, J. D., De Martin, A., Lütge, M., Ferreira, A., Gaudette, B. T., Stanossek, Y., Wang, S., Gonzalez, M. V., Camiolo, E., Wertheim, G., Austin, B., Allman, D., Lim, M. S., Fajgenbaum, D. C., Aster, J. C., Ludewig, B., & Maillard, I. (2023). A novel cryopreservation and biobanking strategy to study lymphoid tissue stromal cells in human disease. bioRxiv : the preprint server for biology, 2023.02.06.525604. https://doi.org/10.1101/2023.02.06.525604
2022
Hoffmann, C., Wechselberger, T., Drexel, H., Dertinger, S., Dirnhofer, S., Pierson, S.K., Fajgenbaum, D.C., & Kessler A. (2022). Idiopathic Multicentric Castleman Disease Occurring Shortly after mRNA SARS-CoV-2 Vaccine. Vaccines (Basel), 10(10), 1725. https://doi.org/10.3390/vaccines10101725
Brandstadter, J.D., & David, C. Fajgenbaum D.C. (2022). How We Manage Idiopathic Multicentric Castleman Disease. Clinical Advances in Hematology Oncology, 20(1), 564-571. http://www.ncbi.nlm.nih.gov/pmc/articles/pmc9584165/
Pierson, S. K., Katz, L., Williams, R., Mumau, M., Gonzalez, M., Guzman, S., Rubenstein, A., Oromendia, A. B., Beineke, P., Fosså, A., van Rhee, F., & Fajgenbaum, D. C. (2022). CXCL13 is a predictive biomarker in idiopathic multicentric Castleman disease. Nature Communications, 13(1), 7236. https://doi.org/10.1038/s41467-022-34873-7
Fajgenbaum, D. C., Pierson, S. K., Kanhai, K., Bagg, A., Alapat, D., Lim, M. S., Lechowicz, M. J., Srkalovic, G., Uldrick, T. S., van Rhee, F., & ACCELERATE Registry Team. (2022). The disease course of Castleman disease patients with fatal outcomes in the ACCELERATE registry. British Journal of Haematology, 198(2), 307–316. https://doi.org/10.1111/bjh.18214
Horna, P., King, R. L., Jevremovic, D., Fajgenbaum, D. C., & Dispenzieri, A. (2022). The lymph node transcriptome of unicentric and idiopathic multicentric Castleman disease. Haematologica. https://doi.org/10.3324/haematol.2021.280370
Wing, A., Xu, J., Meng, W., Rosenfeld, A. M., Li, E. Y., Wertheim, G., Paessler, M., Bagg, A., Frank, D., Tan, K., Teachey, D. T., Lim, M. S., Prak, E. L., Fajgenbaum, D. C., & Pillai, V. (2022). Transcriptome and unique cytokine microenvironment of Castleman disease. Modern Pathology: An Official Journal of the United States and Canadian Academy of Pathology, Inc, 35(4), 451–461. https://doi.org/10.1038/s41379-021-00950-3
Belyaeva, E., Rubenstein, A., Pierson, S. K., Dalldorf, D., Frank, D., Lim, M. S., & Fajgenbaum, D. C. (2022). Bone marrow findings of idiopathic Multicentric Castleman disease: A histopathologic analysis and systematic literature review. Hematological oncology, 40(2), 191–201. https://doi.org/10.1002/hon.2969
Phillips, A. D., Kakkis, J. J., Tsao, P. Y., Pierson, S. K., & Fajgenbaum, D. C. (2022). Increased mTORC2 pathway activation in lymph nodes of iMCD-TAFRO. Journal of cellular and molecular medicine, 26(11), 3147–3152. https://doi.org/10.1111/jcmm.17251
Mukherjee, S., Martin, R., Sande, B., Paige, J. S., & Fajgenbaum, D. C. (2022). Epidemiology and treatment patterns of idiopathic multicentric Castleman disease in the era of IL-6-directed therapy. Blood advances, 6(2), 359–367. https://doi.org/10.1182/bloodadvances.2021004441
Zhang, L., Zhang, M. Y., Cao, X. X., Zhou, D. B., Fajgenbaum, D. C., Dong, Y. J., & Li, J. (2022). A prospective, multicenter study of bortezomib, cyclophosphamide, and dexamethasone in relapsed/refractory iMCD. Leukemia & lymphoma, 63(3), 618–626. https://doi.org/10.1080/10428194.2021.1999437
2021
Goodman, A. M., Jeong, A. R., Phillips, A., Wang, H. Y., Sokol, E. S., Cohen, P. R., Sicklick, J., Fajgenbaum, D. C., & Kurzrock, R. (2021). Novel somatic alterations in unicentric and idiopathic multicentric Castleman disease. European journal of haematology, 107(6), 642–649. https://doi.org/10.1111/ejh.13702
Nishimura, Y., Fajgenbaum, D. C., Pierson, S. K., Iwaki, N., Nishikori, A., Kawano, M., Nakamura, N., Izutsu, K., Takeuchi, K., Nishimura, M. F., Maeda, Y., Otsuka, F., Yoshizaki, K., Oksenhendler, E., van Rhee, F., & Sato, Y. (2021). Validated international definition of the thrombocytopenia, anasarca, fever, reticulin fibrosis, renal insufficiency, and organomegaly clinical subtype (TAFRO) of idiopathic multicentric Castleman disease. American journal of hematology, 96(10), 1241–1252. https://doi.org/10.1002/ajh.26292
Pierson, S. K., Shenoy, S., Oromendia, A. B., Gorzewski, A. M., Langan Pai, R. A., Nabel, C. S., Ruth, J. R., Parente, S. A. T., Arenas, D. J., Guilfoyle, M., Reddy, M., Weinblatt, M., Shadick, N., Bower, M., Pria, A. D., Masaki, Y., Katz, L., Mezey, J., Beineke, P., Lee, D., … Fajgenbaum, D. C. (2021). Discovery and validation of a novel subgroup and therapeutic target in idiopathic multicentric Castleman disease. Blood advances, 5(17), 3445–3456. https://doi.org/10.1182/bloodadvances.2020004016
Lim, J. Y., Duttke, S. H., Baker, T. S., Lee, J., Gambino, K. J., Venturini, N. J., Ho, J. S. Y., Zheng, S., Fstkchyan, Y. S., Pillai, V., Fajgenbaum, D. C., Marazzi, I., Benner, C., & Byun, M. (2021). DNMT3A haploinsufficiency causes dichotomous DNA methylation defects at enhancers in mature human immune cells. The Journal of experimental medicine, 218(7), e20202733. https://doi.org/10.1084/jem.20202733
Koa, B., Borja, A. J., Aly, M., Padmanabhan, S., Tran, J., Zhang, V., Rojulpote, C., Pierson, S. K., Tamakloe, M. A., Khor, J. S., Werner, T. J., Fajgenbaum, D. C., Alavi, A., & Revheim, M. E. (2021). Emerging role of 18F-FDG PET/CT in Castleman disease: a review. Insights into imaging, 12(1), 35. https://doi.org/10.1186/s13244-021-00963-1
Zhang, M. Y., Jia, M. N., Chen, J., Feng, J., Cao, X. X., Zhou, D. B., Fajgenbaum, D. C., Zhang, L., & Li, J. (2021). UCD with MCD-like inflammatory state: surgical excision is highly effective. Blood advances, 5(1), 122–128. https://doi.org/10.1182/bloodadvances.2020003607
Kawano, M., Hara, S., Yachie, A., Inoue, D., Sato, Y., & Fajgenbaum, D. C. (2021). HHV-8-negative multicentric Castleman disease patients with serological, histopathological and imaging features of IgG4-related disease. Rheumatology (Oxford, England), 60(1), e3–e4. https://doi.org/10.1093/rheumatology/keaa362
2020
Abdallah, H., Porterfield, F., & Fajgenbaum, D.C. (2020). Symptomatic relapse and long-term sequelae of COVID-19 in a previously healthy 30-year-old man. BMJ case reports, 13(12), e239825. https://doi.org/10.1136/bcr-2020-239825
Fajgenbaum, D. C., Wu, D., Goodman, A., Wong, R., Chadburn, A., Nasta, S., Srkalovic, G., Mukherjee, S., Leitch, H., Jayanthan, R., Ferrero, S., Sato, Y., Schey, S., Dispenzieri, A., Oksenhendler, E., Zinzani, P. L., Lechowicz, M. J., Hoffmann, C., Pemmaraju, N., Bagg, A., … Castleman Disease Collaborative Network Scientific Advisory Board diagnostic criteria international working group and treatment guidelines international working group (2020). Insufficient evidence exists to use histopathologic subtype to guide treatment of idiopathic multicentric Castleman disease. American journal of hematology, 95(12), 1553–1561. https://doi.org/10.1002/ajh.25992
Fajgenbaum, D. C., & Phillips, A. D. (2020). Commentary on A Case of Rapid Deterioration with Marked Hypergammaglobulinemia. Clinical chemistry, 66(11), 1378–1379. https://doi.org/10.1093/clinchem/hvaa156
Fajgenbaum, D. C., & Rader, D. J. (2020). Teaching Old Drugs New Tricks: Statins for COVID-19?. Cell metabolism, 32(2), 145–147. https://doi.org/10.1016/j.cmet.2020.07.006
Fajgenbaum, D. C., Khor, J. S., Gorzewski, A., Tamakloe, M. A., Powers, V., Kakkis, J. J., Repasky, M., Taylor, A., Beschloss, A., Hernandez-Miyares, L., Go, B., Nimgaonkar, V., McCarthy, M. S., Kim, C. J., Pai, R. L., Frankl, S., Angelides, P., Jiang, J., Rasheed, R., Napier, E., … Pierson, S. K. (2020). Treatments Administered to the First 9152 Reported Cases of COVID-19: A Systematic Review. Infectious diseases and therapy, 9(3), 435–449. https://doi.org/10.1007/s40121-020-00303-8
Pai, R. L., Japp, A. S., Gonzalez, M., Rasheed, R. F., Okumura, M., Arenas, D., Pierson, S. K., Powers, V., Layman, A. A. K., Kao, C., Hakonarson, H., van Rhee, F., Betts, M. R., Kambayashi, T., & Fajgenbaum, D. C. (2020). Type I IFN response associated with mTOR activation in the TAFRO subtype of idiopathic multicentric Castleman disease. JCI insight, 5(9), e135031.
Arenas, D. J., Floess, K., Kobrin, D., Pai, R. L., Srkalovic, M. B., Tamakloe, M. A., Rasheed, R., Ziglar, J., Khor, J., Parente, S. A. T., Pierson, S. K., Martinez, D., Wertheim, G. B., Kambayashi, T., Baur, J., Teachey, D. T., & Fajgenbaum, D. C. (2020). Increased mTOR activation in idiopathic multicentric Castleman disease. Blood, 135(19), 1673–1684. https://doi.org/10.1182/blood.2019002792
Dispenzieri, A., & Fajgenbaum, D. C. (2020). Overview of Castleman disease. Blood, 135(16), 1353–1364. https://doi.org/10.1182/blood.2019000931
Yoshimi, A., Trippett, T. M., Zhang, N., Chen, X., Penson, A. V., Arcila, M. E., Pichardo, J., Baik, J., Sigler, A., Harada, H., Fajgenbaum, D. C., Dogan, A., Abdel-Wahab, O., & Xiao, W. (2020). Genetic basis for iMCD-TAFRO. Oncogene, 39(15), 3218–3225. https://doi.org/10.1038/s41388-020-1204-9
Bernabei, L., Waxman, A., Caponetti, G., Fajgenbaum, D. C., & Weiss, B. M. (2020). AA amyloidosis associated with Castleman disease: A case report and review of the literature. Medicine, 99(6), e18978. https://doi.org/10.1097/MD.0000000000018978
2019
Suarez, A., Reilly, C., & Fajgenbaum, D. C. (2019). Quantitative analysis of a rare disease network's international contact database and E-repository provides insights into biobanking in the electronic consent era. Orphanet journal of rare diseases, 14(1), 173. https://doi.org/10.1186/s13023-019-1145-y
Fajgenbaum, D. C., Langan, R. A., Japp, A. S., Partridge, H. L., Pierson, S. K., Singh, A., Arenas, D. J., Ruth, J. R., Nabel, C. S., Stone, K., Okumura, M., Schwarer, A., Jose, F. F., Hamerschlak, N., Wertheim, G. B., Jordan, M. B., Cohen, A. D., Krymskaya, V., Rubenstein, A., Betts, M. R., … Uldrick, T. S. (2019). Identifying and targeting pathogenic PI3K/AKT/mTOR signaling in IL-6-blockade-refractory idiopathic multicentric Castleman disease. The Journal of clinical investigation, 129(10), 4451–4463. https://doi.org/10.1172/JCI126091
Nabel, C. S., Sameroff, S., Shilling, D., Alapat, D., Ruth, J. R., Kawano, M., Sato, Y., Stone, K., Spetalen, S., Valdivieso, F., Feldman, M. D., Chadburn, A., Fosså, A., van Rhee, F., Lipkin, W. I., & Fajgenbaum, D. C. (2019). Virome capture sequencing does not identify active viral infection in unicentric and idiopathic multicentric Castleman disease. PloS one, 14(6), e0218660. https://doi.org/10.1371/journal.pone.0218660
Kobrin, D. M., Pinto, A. L., Parente, S. T., Gomes, M., Cipriano, M. A., Ribeiro, M. L., & Fajgenbaum, D. C. (2019). Letter to the editor regarding 'Non-cirrhotic portal hypertension associated with multicentric Castleman's disease: a case report'. Acta oncologica (Stockholm, Sweden), 58(4), 515–517. https://doi.org/10.1080/0284186X.2019.1574980
Zhang, L., Zhao, A. L., Duan, M. H., Li, Z. Y., Cao, X. X., Feng, J., Zhou, D. B., Zhong, D. R., Fajgenbaum, D. C., & Li, J. (2019). Phase 2 study using oral thalidomide-cyclophosphamide-prednisone for idiopathic multicentric Castleman disease. Blood, 133(16), 1720–1728. https://doi.org/10.1182/blood-2018-11-884577
Zuccato, M., Shilling, D., & Fajgenbaum, D. C. (2019). The Collaborative Network Approach: a model for advancing patient-centric research for Castleman disease and other rare diseases. Emerging topics in life sciences, 3(1), 97–105. https://doi.org/10.1042/ETLS20180178
Leurs, A., Gnemmi, V., Lionet, A., Renaud, L., Gibier, J. B., Copin, M. C., Hachulla, E., Hatron, P. Y., Launay, D., Fajgenbaum, D.C., & Terriou, L. (2019). Renal Pathologic Findings in TAFRO Syndrome: Is There a Continuum Between Thrombotic Microangiopathy and Membranoproliferative Glomerulonephritis? A Case Report and Literature Review. Frontiers in immunology, 10, 1489. https://doi.org/10.3389/fimmu.2019.01489
Morra, D. E., Pierson, S. K., Shilling, D., Nemat, S., Appiani, C., Guilfoyle, M., Tendler, C., van Rhee, F., & Fajgenbaum, D. C. (2019). Predictors of response to anti-IL6 monoclonal antibody therapy (siltuximab) in idiopathic multicentric Castleman disease: secondary analyses of phase II clinical trial data. British journal of haematology, 184(2), 232–241. https://doi.org/10.1111/bjh.15588
2018
Fajgenbaum D. C. (2018). Novel insights and therapeutic approaches in idiopathic multicentric Castleman disease. Blood, 132(22), 2323–2330. https://doi.org/10.1182/blood-2018-05-848671
van Rhee, F., Voorhees, P., Dispenzieri, A., Fosså, A., Srkalovic, G., Ide, M., Munshi, N., Schey, S., Streetly, M., Pierson, S. K., Partridge, H. L., Mukherjee, S., Shilling, D., Stone, K., Greenway, A., Ruth, J., Lechowicz, M. J., Chandrakasan, S., Jayanthan, R., Jaffe, E. S., … Fajgenbaum, D. C. (2018). International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood, 132(20), 2115–2124. https://doi.org/10.1182/blood-2018-07-862334
Dong, Y., Zhang, L., Nong, L., Wang, L., Liang, Z., Zhou, D., Fajgenbaum, D. C., Ren, H., & Li, J. (2018). Effectiveness of rituximab-containing treatment regimens in idiopathic multicentric Castleman disease. Annals of hematology, 97(9), 1641–1647. https://doi.org/10.1007/s00277-018-3347-0
Baker, T. S., Gambino, K. J., Schriefer, L., Lim, J. Y., Steinberg, K. M., Fajgenbaum, D. C., Martín García-Sancho, A., & Byun, M. (2018). A novel FAS mutation with variable expressivity in a family with unicentric and idiopathic multicentric Castleman disease. Blood advances, 2(21), 2959–2963. https://doi.org/10.1182/bloodadvances.2018023911
Pierson, S. K., Stonestrom, A. J., Shilling, D., Ruth, J., Nabel, C. S., Singh, A., Ren, Y., Stone, K., Li, H., van Rhee, F., & Fajgenbaum, D. C. (2018). Plasma proteomics identifies a 'chemokine storm' in idiopathic multicentric Castleman disease. American journal of hematology, 93(7), 902–912. https://doi.org/10.1002/ajh.25123
Lee, J., Werth, V. P., Hall, R. P., 3rd, Eming, R., Fairley, J. A., Fajgenbaum, D. C., Harman, K. E., Jonkman, M. F., Korman, N. J., Ludwig, R. J., Murrell, D. F., Musette, P., Naik, H. B., Sadik, C. D., Yamagami, J., Yale, M. L., & Payne, A. S. (2018). Perspective From the 5th International Pemphigus and Pemphigoid Foundation Scientific Conference. Frontiers in medicine, 5, 306. https://doi.org/10.3389/fmed.2018.00306
Fajgenbaum, D. C., & Shilling, D. (2018). Castleman Disease Pathogenesis. Hematology/oncology clinics of North America, 32(1), 11–21. https://doi.org/10.1016/j.hoc.2017.09.002
Soudet, S., Fajgenbaum, D.C., Delattre, C., Forestier, A., Hachulla, E., Hatron, P. Y., Launay, D., & Terriou, L. (2018). Schnitzler syndrome co-occurring with idiopathic multicentric Castleman disease that responds to anti-IL-1 therapy: A case report and clue to pathophysiology. Current research in translational medicine, 66(3), 83–86. https://doi.org/10.1016/j.retram.2018.06.001
2017
Louis, C., Vijgen, S., Samii, K., Chalandon, Y., Terriou, L., Launay, D., Fajgenbaum, D. C., Seebach, J. D., & Muller, Y. D. (2017). TAFRO Syndrome in Caucasians: A Case Report and Review of the Literature. Frontiers in medicine, 4, 149. https://doi.org/10.3389/fmed.2017.00149
Srkalovic, G., Marijanovic, I., Srkalovic, M. B., & Fajgenbaum, D. C. (2017). TAFRO syndrome: New subtype of idiopathic multicentric Castleman disease. Bosnian journal of basic medical sciences, 17(2), 81–84. https://doi.org/10.17305/bjbms.2017.1930
Yu, L., Tu, M., Cortes, J., Xu-Monette, Z. Y., Miranda, R. N., Zhang, J., Orlowski, R. Z., Neelapu, S., Boddu, P. C., Akosile, M. A., Uldrick, T. S., Yarchoan, R., Medeiros, L. J., Li, Y., Fajgenbaum, D. C., & Young, K. H. (2017). Clinical and pathological characteristics of HIV- and HHV-8-negative Castleman disease. Blood, 129(12), 1658–1668.
Fajgenbaum, D. C., Uldrick, T. S., Bagg, A., Frank, D., Wu, D., Srkalovic, G., Simpson, D., Liu, A. Y., Menke, D., Chandrakasan, S., Lechowicz, M. J., Wong, R. S., Pierson, S., Paessler, M., Rossi, J. F., Ide, M., Ruth, J., Croglio, M., Suarez, A., Krymskaya, V., … Lim, M. S. (2017). International, evidence-based consensus diagnostic criteria for HHV-8-negative/idiopathic multicentric Castleman disease. Blood, 129(12), 1646–1657. https://doi.org/10.1182/blood-2016-10-746933
Behnia, F., Elojeimy, S., Matesan, M., & Fajgenbaum, D. C. (2017). Potential value of FDG PET-CT in diagnosis and follow-up of TAFRO syndrome. Annals of hematology, 96(3), 497–500. https://doi.org/10.1007/s00277-016-2875-8
2016
Liu, A. Y., Nabel, C. S., Finkelman, B. S., Ruth, J. R., Kurzrock, R., van Rhee, F., Krymskaya, V. P., Kelleher, D., Rubenstein, A. H., & Fajgenbaum, D. C. (2016). Idiopathic multicentric Castleman's disease: a systematic literature review. The Lancet. Haematology, 3(4), e163–e175. https://doi.org/10.1016/S2352-3026(16)00006-5
Fajgenbaum, D. C., Ruth, J. R., Kelleher, D., & Rubenstein, A. H. (2016). The collaborative network approach: a new framework to accelerate Castleman's disease and other rare disease research. The Lancet. Haematology, 3(4), e150–e152. https://doi.org/10.1016/S2352-3026(16)00007-7
Iwaki, N., Fajgenbaum, D. C., Nabel, C. S., Gion, Y., Kondo, E., Kawano, M., Masunari, T., Yoshida, I., Moro, H., Nikkuni, K., Takai, K., Matsue, K., Kurosawa, M., Hagihara, M., Saito, A., Okamoto, M., Yokota, K., Hiraiwa, S., Nakamura, N., Nakao, S., … Sato, Y. (2016). Clinicopathologic analysis of TAFRO syndrome demonstrates a distinct subtype of HHV-8-negative multicentric Castleman disease. American journal of hematology, 91(2), 220–226. https://doi.org/10.1002/ajh.24242
Fajgenbaum, D. C., & Kurzrock, R. (2016). Siltuximab: a targeted therapy for idiopathic multicentric Castleman disease. Immunotherapy, 8(1), 17–26. https://doi.org/10.2217/imt.15.95
2015
Newman, S. K., Jayanthan, R. K., Mitchell, G. W., Carreras Tartak, J. A., Croglio, M. P., Suarez, A., Liu, A. Y., Razzo, B. M., Oyeniran, E., Ruth, J. R., & Fajgenbaum, D. C. (2015). Taking Control of Castleman Disease: Leveraging Precision Medicine Technologies to Accelerate Rare Disease Research. The Yale journal of biology and medicine, 88(4), 383–388.
2014
Fajgenbaum, D. C., van Rhee, F., & Nabel, C. S. (2014). HHV-8-negative, idiopathic multicentric Castleman disease: novel insights into biology, pathogenesis, and therapy. Blood, 123(19), 2924–2933. https://doi.org/10.1182/blood-2013-12-545087
Fajgenbaum, D. C., Rosenbach, M., van Rhee, F., Nasir, A., & Reutter, J. (2013). Eruptive cherry hemangiomatosis associated with multicentric Castleman disease: a case report and diagnostic clue. JAMA dermatology, 149(2), 204–208. https://doi.org/10.1001/jamadermatol.2013.1552
-

Meet the Team
We are an interdisciplinary mix of clinical data analysts, cell biologists, lab technicians, physicians, and data scientists.
-

Our Research
We utilize a number of technologies and techniques to answer questions about Castleman Disease and other cytokine storm disorders.
-

Keep Up With Recent News in the Lab
With so many moving pieces, it’s often difficult to keep up with everything going on in our Center!
-

Join us
Interested in joining the CSTL? See what positions/opportunities we currently have available!







